Another budget has come around and often what I wish is that we could just fulfil all the requests and suggestions that many of us have made and written about for all the past budgets.
The Budget 2024 allocation for healthcare was RM41.2 billion; 10.46% of the total budget and second highest after the Education Ministry.
Although this looks large, it is not able to support the growth we need in our ailing health services.
For far too long we have neglected our health services and hence any small increment in budget is swallowed up in the enormous needs and challenges our health services face.
One problem of not sufficiently funding our health services over the decades, is that we have not adequately developed services for children and pregnant women while now facing the enormous burden of NCDs, psycho-social health, disability and the elderly. And therein lies the rub, the quandary.
We have a limited pie, limited resources. Where do we invest it? The needs and challenges are enormous. Hence a critical request is that we consider two budgets for the Ministry of Health.
One, the usual healthcare budget with annual increments. But in addition, a large supplementary budget, specifically to fix our health service challenges.
We will need to provide this supplementary budget for a number of years.
Of course, it will be said we do not have the money to do this but we can stop funding some unnecessary areas and keep our focus on health, education, welfare and economic areas.
If we do not do this, then we cannot expect our sickly health services to improve, let alone reach inner-city poor, rural Sabah and the indigenous; all of whom currently have limited healthcare access and services. Not to mention the decaying, old hospitals and equipment; some of which are fire hazards.
We need the supplementary budget to address multiple urgent health care needs and develop services appropriate for them.
The key of course is to invest in prevention and community services – by community I do not mean public health services but true services in the community.
Only if we move ‘upstream’ to stop the enormous burden of disease that is developing downstream can we stamp this never-ending burden of physical diseases (the NCDs).
Some areas often get more funding because most of our clinicians are trained in disease rather than health.
We no longer run a Ministry of Health but a Ministry of Disease. Hence, we focus on chronic illnesses and invest in dialysis, coronary disease, stroke, etc.
All these are important but are ever growing and never-ending issues unless we deal with prevention.
The Budget needs to invest and develop care in the community.
Governments are more interested in ‘jam today’ as it is good for winning elections, while ‘jam tomorrow’ takes many years to bear fruit and is hence not politically expedient.
This is the weakest link in our current healthcare services – we have not grown the capacity of the community to better deal with their own health but instead focused on an addiction to a curative, specialist and drug-based illness system.
Community health services should be mobile (bus-based) rather than static (building-base), they should be decentralised, utilise adequate community health (nursing-based trained) and trans-disciplinary workers (disability, elderly, adolescent-mental health trained), and use civil society organisations (CSOs) better.
The focus should be on empowering the community for self-care and training/supporting care partners.
Our urban, inner-city health services are poor and 75% of all Malaysians live in urban settings.
These mobile health services can outreach to the urban, inner-city poor, to the disabled, to the elderly, to the single mother, the pregnant and young children.
I hope Budget 2025 will be a humane one focusing on the health, education, welfare and economic needs of the poor and middle class – the B60.
There are no health services without health personnel and we have not supported our healthcare staff adequately in terms of financial remuneration, resources to do the work, creating a meaningful work environment and reducing their workload.
The Budget must address this current staffing crisis, not just for doctors but also for nurses, pharmacists and other allied healthcare staff.
If we do not address retention of healthcare professionals, provide clear pathways for specialisation, and deal with wide-spread burnout due to workload, we will continue to have a weakened health service.
Finally, as a paediatrician, I am appalled by the continued lack of investment in services for children; we do not really care for our children no matter what we say.
The budget for paediatric services has shrunk relative to the total budget (1.5% of total health budget in 2024 compared to 1.7% in 2023 and 2.2% in 2020).
Our intensive care service available for babies and children is one of the poorest for the region.
This must stop. We cannot keep denying ill children the neonatal and paediatric intensive care beds they so desperately need.
This is reflected in all our child mortality indicators that have been stagnant for more than 20 years.
Many decades ago, I read an economic research article entitled “Jam Today vs Jam Tomorrow”.
It argued that governments are more interested in ‘jam today’ which is curative health services as it was good for winning elections.
‘Jam tomorrow’, investing in prevention and the community, would take many years to bear fruit and hence not politically expedient.
I hope Budget 2025 will reverse this trend for health. It does not matter if you do not win elections.
What matters is investing in the right and meaningful actions and sowing the seeds for a better tomorrow for our beloved nation.
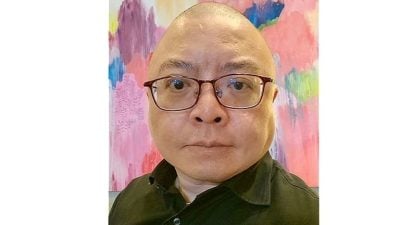
(Dato’ Dr Amar-Singh HSS is Consultant Paediatrician, Child-Disability Activist.)
ADVERTISEMENT
ADVERTISEMENT