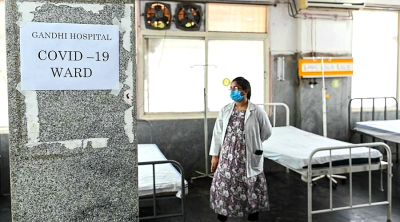
As Malaysia1 and most of the world transitioned to the endemic phase of COVID-19, it’s easy to forget that just two years ago, the pandemic had led to millions of lives lost, rise in unemployment rates and the near-collapse of healthcare systems due to the tsunami of cases.
Today, thanks to the quick development of medical innovations such as COVID-19 vaccines, we are now able to continue living our lives in the new normal, resuming productivity and building towards economic recovery and growth.
Now that we have seen the long-lasting and devastating impact that a pandemic can leave, it is vital that we draw our attention to tackling another urgent public health crisis – antimicrobial resistance (AMR) which continues to rise to alarming levels across the world2.
To put things into perspective, at the height of the pandemic, we were still fighting against newer COVID-19 variants, and many were unsure if current vaccines and therapeutics were effective in combating them3.
This stresses the importance of continuing to innovate and developing new and effective ways to combat microorganisms including viruses, bacteria and fungi as they change and mutate4 over time.
AMR – the silent pandemic we should all know about
Over the years, antimicrobial resistance has become an urgent health challenge on a global scale, as microbes such as bacteria, fungi and viruses no longer respond to commonly used medicines, resulting in infections becoming harder to treat.
With drug resistance, antimicrobial treatment no longer serves their desired effects, which in turn will increase the risk of poor outcomes in patients with an infection caused by AMR5.
During the COVID-19 pandemic, there was a significant increase in antibiotic prescriptions despite a relatively low bacterial co-infection rate.
The misuse of antibiotics in these patients can result in increased selective pressure for antimicrobial resistance leading to a lasting consequence of the COVID-19 pandemic6.
Apart from overprescribing of antibiotics unnecessarily, the increased risk of AMR is compounded by the lack of awareness of appropriate antibiotic use and a poor understanding of the consequences of misusing antibiotics among the public7.
It is estimated that drug resistance claims 700,000 lives every year, and this toll is projected to increase exponentially to 10 million a year by 2050 without immediate action8.
The unchecked growth of drug-resistant infections has allowed for AMR to become a slow-moving pandemic that requires urgent attention as it will have long-term consequences for the global public health and economy.
Impacts on the lack of new antibiotics to fight AMR is a cause for concern
Before the discovery of antibiotics in the 20th century, contracting even a mild infection could result in the loss of life or significant morbidity such as loss of a limb.
The discovery of antibiotics was a turning point in human history, revolutionizing medicine and increasing the survival rates of infected patients over time.
However, the growing burden of AMR threatens the return to a world with a scarcity of effective treatments for patients who have common bacterial infections such as urinary tract infection, pneumonia, skin infection and surgical site infections.
As the effects of AMR continue to increase today, the antibiotic pipeline is slowing down, and the discovery and development of new antimicrobials is not able to keep up against the emergence of AMR.
In 2019, the WHO had identified 32 antibiotics in clinical development which address its list of priority pathogens, however, only six were classified as innovative9.
This is indicative of two things – firstly, the research and development of new antibiotics is a lengthy and complex process that doesn’t happen overnight; and secondly, more needs to be done to address the clinical pipeline of new antimicrobials to ensure that patients are able to receive the care that they need.
At this juncture, antibiotics have become more ineffective as the global spread of drug resistance has made it difficult to treat infections and increasing the risk of death10.
This is why there is an urgent need for new antibacterial drugs in the market, but with this comes the importance of ensuring that these antibiotics are used wisely.
Patients should be prescribed antibiotics only when needed at the right dose, frequency and duration, otherwise the new antibiotics will also suffer the same fate as their predecessors and eventually lose effectiveness11.
Additionally, the cost of AMR to national economies and their health systems is another crucial factor to note, as it can result in productivity loss caused by sickness and premature death, as well as rise in healthcare cost that stems from prolonged hospital stays and care12.
Without effective tools for the prevention and adequate treatment of drug-resistant infections, treatment may fail for an increasing number of patients.
There will also be an increased risk in major medical procedures such as surgery, chemotherapy and organ transplants13.
Steps we can take to prevent/reduce AMR
Understanding the devastating effects of AMR, we must now take the first steps in acknowledging that it is a complex problem that requires a united multisectoral approach.
As patients are the end consumers of medical treatments including users of antibiotics, they play an important role in how the AMR situation will progress in the coming years.
Patients should only take antibiotics prescribed by a doctor and they must correctly follow the prescription directions.
The public should also refrain from demanding for antibiotics and buying medication without a prescription, on top of sharing or taking leftover antibiotics14.
To continue raising awareness, our healthcare professionals must also play a more proactive role in educating and guiding their patients, to ensure they have the capacity to benefit from healthcare while prescribing antibiotics to patients only when required so that they are being used correctly.
Apart from judicious antibiotic use, maintaining strict infection prevention measures such as hand hygiene reduces the spread of AMR organisms in healthcare settings as well as in the community15.
Additionally, vaccinations also play an important role in combating AMR.
There is now increasing evidence that certain vaccines currently available such as influenza16, pneumococcus17, rotavirus, Hemophilus influenza18 can decrease the risks of AMR by preventing bacterial and viral infections.
This would mean that consumers, particularly children and elderlies19 who keep up to date on their vaccination schedules may be able to reduce the use of antibiotics, and thus prevent antibiotic-resistant infections20.
Besides creating awareness among consumers and healthcare professionals, combating AMR also requires action from governments, policymakers and industry players to really address the crux of the issue.
Investment is required in antibiotic research and development, both as a tool to control novel disease outbreaks and to treat known pathogens developing resistance to currently available treatments.
Although it might take time before we can curb the issue of AMR in Malaysia and across the globe, if we are committed to playing our parts, it is a goal that we can achieve together.
We must learn from the COVID-19 pandemic to address the next global and public health threat.
We have seen that it is indeed possible for all parties to work together to reduce the spread of COVID-19 – from citizens adhering to new SOPs, pharmaceutical companies driving innovations that led to the creation of vaccines and COVID-19 treatment, and governments which put in place and enforced guidelines for the people while also supporting the R&D of these innovations.
With AMR, the same urgency is needed so that we can prevent the next public health crisis.
Footnotes:
1. MYSOP. Standard Operating Procedure (SOP) #ReopeningSafely [cited 2022 May 25]
2. WHO. Antibiotic resistance [cited 2022 Apr 15]
3. Mayo Clinic. Do COVID-19 vaccines protect against the variants? [cited 2022 June 20]
4. Centers for Disease Control and Prevention (CDC). Variants of the Virus
5. Francesca Prestinaci, Patrizio Pezzotti, Annalisa Pantosti. Antimicrobial resistance: a global multifaceted phenomenon [cited 2022 Apr 15]
6. Langford, Bradley J., et al. “Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis.” Clinical microbiology and infection 27.4 (2021): 520-531.
7. Wong, Li Ping, et al. “Factors influencing inappropriate use of antibiotics: Findings from a nationwide survey of the general public in Malaysia.” PloS one 16.10 (2021): e0258698
8. The World Bank. Antimicrobial Resistance (AMR) [cited 2022 May 25]
9. WHO. 2019 Antibacterial agents in clinical development: an analysis of the antibacterial clinical development pipeline [cited 2022 May 25]
10. WHO. Antibiotic resistance [cited 2022 Apr 15]
11. Mayo Clinic. Antibiotics: Are you misusing them? [cited 2022 Apr 15]
12. Porooshat Dadgostar. Antimicrobial Resistance: Implications and Costs [cited 2022 Apr 15]
13. WHO. Antibiotic resistance [cited 2022 Apr 15]
14. WHO. Raising awareness and educating on antimicrobial resistance [cited 2022 Apr 15]
15. Hong Kong Strategy and Action Plan on Antimicrobial Resistance 2017-2022 [cited 2022 Nov 15]
16. Kwong JC, et al. Clin Infect Dis. “The effect of universal influenza immunization on antibiotic prescriptions: an ecological study.” 49:750-6 (2009).
17. Lewnard, J.A., Nature, C.L., et al. “Childhood vaccines and antibiotic use in low- and middle-income countries.” 581, 94–99 (2020).
18. Palmu, Arto A., et al. “Effect of pneumococcal Hemophilus influenzae protein D conjugate vaccine (PHiD-CV10) on outpatient antimicrobial purchases: a double-blind, cluster randomized phase 3–4 trial.” 14.3: 205-212 (2014).
19. Nichol KL, et al. N Engl J Med. “Effectiveness of Influenza Vaccine in the Community-Dwelling Elderly.” 357:1373-1381 (2007).
20. Kingwell. Nat Rev Drug Discov. “Vaccines take a shot at antimicrobial resistance.” 17, 229–231 (2018).
(Prof Dr. Sasheela a/p Sri La Sri Ponnampalavanar is Infectious Disease Professor at Universiti Malaya Medical Center, UMMC.)
ADVERTISEMENT
ADVERTISEMENT