By Dr Nur Nabila binti Nasharuddin / Dr Khor Swee Kheng
The COVID-19 pandemic has caused more than 1,700 deaths and 445,000 cases in Malaysia so far (as of 10 May 2021).
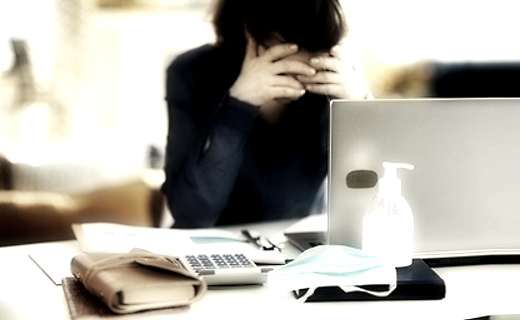
Beyond the staggering numbers, this pandemic is also causing a significant mental health crisis that is even more palpable after a year.
As Malaysia starts MCO 3.0, we must act now to prevent a mental health crisis precipitated by MCO 3.0.
In this article, we share three sobering statistics to demonstrate the impact of COVID-19 and MCOs on mental health in Malaysia, provide three reasons why mental health is deteriorating, and propose three systemic solutions to improve our mental health infrastructure in Malaysia for this pandemic.
In statistical terms, the effects of the COVID-19 pandemic have been stark. A study of 1,163 respondents by Universiti Malaya showed a consistent increase in the prevalence of depression, anxiety and stress symptoms across four different Movement Control Orders (MCO) in Malaysia.
The highest rates of depression and anxiety symptoms were recorded at 59.2% and 55.1% respectively, between August to September 2020.
The Malaysian Mental Health Association (MMHA) recorded a more than two-fold increase in people seeking help related to stress throughout 2020 compared to 2019.
In 2020, one in three calls that Befrienders received were suicidal in nature, as compared to one out of ten calls in 2018.
The government's psychosocial hotline recorded 37,709 calls between April and September 2020, half of them related to emotional distress worsened by the pandemic and MCO.
These statistics are sobering and indicate a deterioration of mental health over time.
There are three systemic reasons why the mental health landscape has deteriorated.
Firstly, the pandemic has drawn resources away from mental health care towards pandemic care.
According to a Ministry of Health report in 2016, the scale for people with mental health conditions has been tipped well before COVID-19, but this pandemic worsens it.
With more resources concentrated on the pandemic, less acute services like mental healthcare facilities are displaced. Access to psychiatric services like walk-in appointments or hospital visits is drastically reduced during the pandemic, to adhere to the social distancing measures. This is worsened by the geographical maldistribution of psychiatric services in Malaysia.
Secondly, mental health is worsened by the rapid changes brought by the pandemic, including MCOs, isolation and social distancing.
The public are affected by sudden and prolonged uncertainty brought by the pandemic, and this amplifies their anxiety, depression and fear of illness.
Besides clear disruption of daily activities, MCOs also compound other factors like enforced separation from family and friends.
Furthermore, exposure to fake news and disinformation regarding COVID-19 and vaccinations increase anxiety and fear. The younger generations are evidently more affected, with more than half respondents from the age of 18 to 34 reporting worse mental well-being in 2021 compared to 2020, as reported by The Centre.
Thirdly, loss of livelihoods predisposes the individual to mental stress.
The economic repercussion of COVID-19 pandemic is widespread and deep. The unemployment rate was 4.9% in January 2021, much higher than the 3.2% rate recorded in January 2020. Financial hardship, unemployment and lower socioeconomic status are risk factors to develop mental health conditions.
The impact of the COVID-19 outbreak on the livelihood of the lower-income group are extreme, worsened by the inability to maintain nutrition, subsistence and their physical welfare. All of this causes an increase in anxiety, depression or mental health conditions.
We would like to propose three systemic solutions to avert an imminent mental health crisis, precipitated by MCO 3.0.
Our first systemic solution is in the risk communications of the public health response to COVID-19. It should provide clear, concise and accurate information about quarantine, infection rates, healthcare capacity and vaccination rollout.
Health communication in a dynamic situation like this should signal confidence and honesty, to reduce uncertainty in the population.
An organized and standardized national approach to COVID-19 management is paramount to improve the citizens' sense of coherence and manageability, which are major sources of resilience.
Our second systemic solution is in the mental healthcare system, which needs to be expanded and be more resilient to manage this crisis.
Easier access to mental healthcare, including widespread use of telehealth for services like counseling, psychotherapy, medication management and vocational interventions should be developed.
It is important to develop the needed digital infrastructure and regulations that enable the digital health framework and delivery.
Task shifting, a process of delegation where tasks are moved from highly-specialized to less-specialized health workers, has been proven to be beneficial especially in low-resource areas.
Upskilling the current workforce in mental health services and delivery is another useful strategy, especially when there are multiple avenues in Malaysia, including the private, non-governmental and civil society avenues.
Access to courses like Mental Health First Aid can be subsidized to increase its reach to the general population, and to perhaps have a "Counsellor in Every Community" project.
Our final systemic solution to strengthen mental health in Malaysia is to strengthen the social protection and wage support system to address the risk factors of mental health issues.
Urgent, targeted and flexible measures to support vulnerable groups like those in the informal economy and areas highly affected by the pandemic should be implemented with frameworks and benchmarks from international labor standards.
Cash transfers programs like Bantuan Prihatin Nasional have been implemented as a part of social protection method, but long-term recovery plan should be crafted to maximize the economic impact of such stimulus.
Besides, maintenance of food security in areas with restricted access can be improved with the help of local government, which can be more responsive than the federal government as they are closer to the ground.
To conclude, the mental health effects of COVID-19 are massive and mitigating them is a national public health priority.
The increase of COVID-19 cases in the recent months makes it easy to overlook the invisible mental health aspect of this pandemic, but this unseen crisis can be catastrophic and can worsen the physical pandemic of COVID-19.
The right government policy responses are needed to save Malaysians from the mental anguish that COVID-19 is causing. We must act now to avert a mental health crisis.
ADVERTISEMENT
ADVERTISEMENT


































