With a surge of Covid-19 spreading rapidly across China after the “zero Covid policy” was abandoned, the newly appointed minister of health Dr Zaliha Mustafa, herself a medical practitioner, advocated as many people as possible go and get a Covid-19 booster immediately.
Ministry of health director general Dr Noor Hisham announced to the press that 96.5 percent of 298 wastewater samples taken at airports over the last six months were found to be contaminated with Covid-19.
This means the majority of people entering Malaysia by air were carriers of, or exposed to Covid-19.
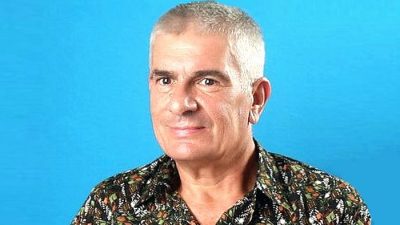
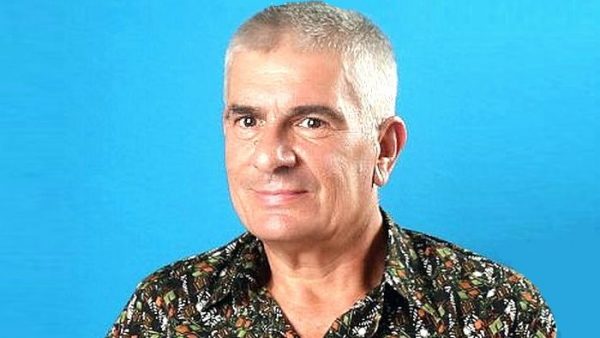
Nevertheless, Dr Zaliha ordered a stepping up of Covid-19 SOPs whereby people coming into Malaysia would need to show they were Covid-free, in an attempt to stem the spread of the BA5.2 and BF7 variants now circulating in China.
There are already 4,148 cases infected with BA5.3 and three cases of BF.7 in Malaysia as of 31st December. This can be expected to exponentially rise in the near future.
Dr Zaliha handled her first emergency as most other health ministers around the world have handled it. However, emerging research is showing the risk/benefit ratios of vaccines are now vastly different from 2021, and airport screening will do very little or nothing to stem the flow of the new Chinese variants coming into the country. They are already here!
The hope for Malaysia is that in China, the draconian lockdowns prevented citizens developing immunity, hence the rapid increase in cases once lockdowns were dispensed with.
Levels of immunity are much higher in Malaysia due to previous outbreaks, and high levels of vaccination should protect the local population from a similar outbreak like China is currently experiencing.
This outbreak in China should not distract the new minister away from other potential crises facing the Malaysian health system. Much needed focus and resources are required in other areas.
Need to move away from Covid-centric focus
Covid-19 is not the only infectious disease epidemic Malaysia is facing now. Influenza, and Respiratory Syncytial Virus (RSV) are also spreading around the community, which can have dire effects upon the young and vulnerable.
Dengue fever is expected to be at epidemic levels over the next three years, potentially fatal to the vulnerable.
This is not to mention the traditional causes of death including ischemic heart disease, pneumonia, cerebrovascular diseases, road accidents, diabetes, malignant neoplasm of the respiratory system, hypertensive diseases, chronic lower respiratory diseases, and malignant neoplasm of the colon, rectum and anus.
These disorders are killing many more people than what Covid is expected to kill over the next year.
Brain drain
Medical brain drain of doctors and other specialized personnel is a symptom of the contract system.
Doctors are given contracts which delay any permanent appointment to a hospital. This takes away any career path certainty, a dual salary and benefits system prejudiced against contract doctors, double standards by administrators, and overwork in a poor institutional environment.
This is pushing doctors and other medical specialists to nearby Singapore, Australia and the UK.
This continued brain drain could potentially cripple the public health system with shortages of competent medical personnel.
Lack of focus upon mental health
The public health system is orientated towards treating physical ailments where mental health is grossly underfunded.
Suicides have dramatically risen over the last three years with a chronic shortage of psychiatrists, psychologists and counselors. There are often long waiting periods for the few who are available.
Issues of stress, depression and various forms of neurosis are overlooked within an overworked public health system.
A need for programs to encourage general health well–being
Preventative health is almost totally ignored. There are no coordinated educational programs to assist the community to avoid poor health.
Social and environmental factors that can lead to heart issues, obesity and diabetes are not being tackled, leading to a society with poor general health.
Programs concerned with diet, nutrition and exercise could lead to a much healthier society with better community immune to many general diseases.
Equipment and infrastructure
Spending on public health must be increased immediately, rather than just planned.
Lack of equipment and infrastructure is leading to overcrowded emergency and trauma facilities, wards and outpatient facilities.
Plans for new hospital expansion is far behind rapid urbanization. Hospitals in most towns and cities are too small for demand, which is increasing due to an aging population.
This issue has been mentioned by the Auditor-General in a number of annual reports. The recent Covid pandemic highlighted the lack of hospital capacity, particularly with infectious diseases. This should be the most important lesson from the pandemic.
There needs to be a rapid upgrading in diagnostic equipment, training and expertise. Public dental facilities are not adequate and out of reach to many in remote locations.
Universal insurance
Public health is currently free for all citizens. However, there needs to be some form of universal insurance scheme, perhaps based upon tax to fund the public health system in future.
This can be used for specified services that hospitals can fund on a fee basis. This issue will need to be considered in the long-term to assist the growth, standards and expansion of the public health service.
Medical costs will become the most expensive household item in the near future.
Medical malpractice
Medical malpractice, like in all other countries, is a major issue of concern.
Much medical malpractice goes totally unreported, where remedies to patients’ injuries go unrecorded.
According to the ministry of health’s official, medical malpractice has risen dramatically over the last few years. Cases involving wrongful surgery, unintended retention of foreign objects and falls while in hospital reached nearly 10,000 cases in 2020.
Patients most often suffer in silence, where the ministry of health, Malaysia Medical Council (MMC) are not complaint-friendly.
Taking these cases to court is very expensive, where many lawyers won’t take on such cases as success rates are very low.
There is a massive challenge ahead for the new minister. Let’s hope screening for Covid-19 at airports and placing sanitary napkins in ministry toilets doesn’t take away from the other jobs that need to be done to make the public health system what it should be for Malaysians.
(Murray Hunter has been involved in Asia-Pacific business for the last 40 years as an entrepreneur, consultant, academic and researcher. He was an associate professor at Universiti Malaysia Perlis.)
ADVERTISEMENT
ADVERTISEMENT